From Centaurus to XBB: your handy guide to the latest COVID subvariants (and why some are more worrying than others)
Written by Dr Sebastian Duchene, ARC DECRA Research Fellow and Dr Ash Porter, CDGN VoC Working Group Member and Research Officer at the Doherty Institute
From Centaurus to XBB: your handy guide to the latest COVID subvariants (and why some are more worrying than others)
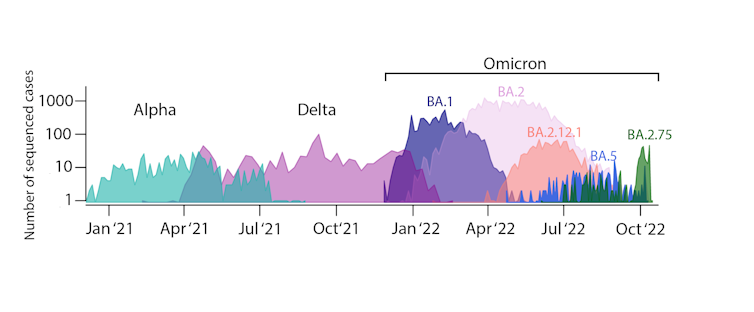
Ash Porter, The Peter Doherty Institute for Infection and Immunity and Sebastian Duchene, The University of MelbourneThe Omicron variant of concern has splintered into multiple subvariants. So we’ve had to get our heads around these mutated forms of SARS-CoV-2, the virus that causes COVID-19, including BA.1 and the more recent BA.5.
We’ve also seen recombinant forms of the virus, such as XE, arising by genetic material swapping between subvariants.
More recently, XBB and BQ.1 have been in the news.
No wonder it’s hard to keep up.
The World Health Organization (WHO) has had to rethink how it describes all these subvariants, now labelling ones we need to be monitoring more closely.
What’s the big deal with all these subvariants?
Omicron and its subvariants are still causing the vast majority of COVID cases globally, including in Australia.
Omicron subvariants have their own specific mutations that might make them more transmissible, cause more severe disease, or evade our immune response.
Omicron and its subvariants have pushed aside previous variants of concern, the ones that led to waves of Alpha and Delta earlier in the pandemic.
Now, in Australia, the main Omicron subvariants circulating are BA.2.75, and certain versions of BA.5. More on these later.
We still don’t fully understand the driving forces behind the emergence and spread of certain SARS-CoV-2 subvariants.
We can, however, assume the virus will keep evolving, and new variants (and subvariants) will continue to emerge and spread in this wave-like pattern.
How do we keep track of this all?
To monitor these subvariants, the WHO has defined a new category, known as “Omicron subvariants under monitoring”.
These are ones that have specific combinations of mutations known to confer some type of advantage, such as being more transmissible than others currently circulating.
Researchers and health authorities keep track of circulating subvariants by sequencing the genetic material from viral samples (for instance, from PCR testing or from wastewater sampling). They then upload the results to global databases (such as GISAID) or national ones (such as AusTrakka).
These are the Omicron subvariants authorities are keeping a closer eye on for any increased risk to public health.
Newer versions of BA.5
The BA.5 subvariant that arose in early February 2022 is still accumulating more mutations.
The WHO is monitoring BA.5 versions that carry at least one of five additional mutations (known as S:R346X, S:K444X, S:V445X, S:N450D and S:N460X) in the spike gene.
The spike gene codes for the part of the virus that recognises and fuses with human cells. We are particularly concerned about mutations in this gene as they might increase the virus’ ability to bind with human cells.
Throughout recent months, BA.5 has been the dominant subvariant in Australia. However, BA.2.75 has now established a foothold.
BA.2.75 or Centaurus
The BA.2.75 subvariant, sometimes called Centaurus, was first documented in December 2021. It possibly emerged in India, but has been detected around the globe.
This includes in Australia, where more than 400 sequences have been uploaded to the GISAID database since June 2022.
This subvariant has up to 12 mutations in its spike gene. It seems to spread more effectively than BA.5. This is probably due to being better able to infect our cells, and avoiding the immune response driven by previous infection with other variants.
BJ.1
This was first detected in early September 2022 and has a set of 14 spike gene mutations.
It has mostly been detected in India or in infections coming from this area.
We know very little about the impact of its mutations and at the time of writing, there was only one Australian sequence reported.
BA.4.6 or Aeterna
BA.4.6, sometimes called Aeterna, was detected in January 2022 and has been spreading rapidly in the United States and the United Kingdom.
There have been more than 800 sequences uploaded to the GISAID database in Australia since May 2022.
It may be more easily transmitted from one person to the next due to its spike gene mutations.
Early data suggests it is better able to resist cocktails of therapeutic antibodies compared with BA.5. This makes antibody therapies, such as Evusheld, less effective against it.
BA.2.3.20
This was first detected in the US in August 2022. It has a set of nine mutations in the spike gene, including a rare double mutation (A484R).
Like BA.2.75, this subvariant is probably better able to infect our cells and avoid the immune response driven by previous infection.
There are more than 100 Australian genomic sequences reported in the GISAID database, all from August 2022.
XBB
This recombinant version of the virus was detected in August 2022. It is a result of the swapping of genetic material between BA.2.10.1 and BA.2.75. It has 14 extra mutations in its spike gene compared with BA.2.
Although there have only been 50 Australian genomic sequences reported in GISAID since September, we anticipate cases will rise. Lab studies indicate therapeutic antibodies don’t work so well against it, with XBB showing strong resistance.
Although XBB appears to be able to spread faster than BA.5, there’s no evidence so far it causes more severe disease.
How about BQ.1?
Although it is not on the WHO list of subvariants under monitoring, cases of the BQ.1 subvariant are rising in Australia. BQ.1 contains mutations that help the virus evade existing immunity. This means infection with other subvariants, including BA.5, may not protect you against BQ.1.
In the meantime, your best protection against severe COVID, whichever subvariant is circulating, is to make sure your booster shots are up-to-date. Other ways to prevent SARS-CoV-2 infection include wearing a fitted mask, avoiding crowded spaces with poor ventilation, and washing your hands regularly. ![]()
Ash Porter, Research officer, The Peter Doherty Institute for Infection and Immunity and Sebastian Duchene, Australian Research Council Future Fellow, The University of Melbourne
This article is republished from The Conversation under a Creative Commons license. Read the original article.

